A high court judge has ruled that the National Health Service has responsibility for deciding whether or not to supply a drug called PrEP that helps prevent the transmission of HIV, the virus that causes AIDS.
The decision has been hailed as a victory by gay campaigners. But others argue that the NHS should be spending its scarce resources on what they regard as much more urgent and deserving treatments. Who is right?
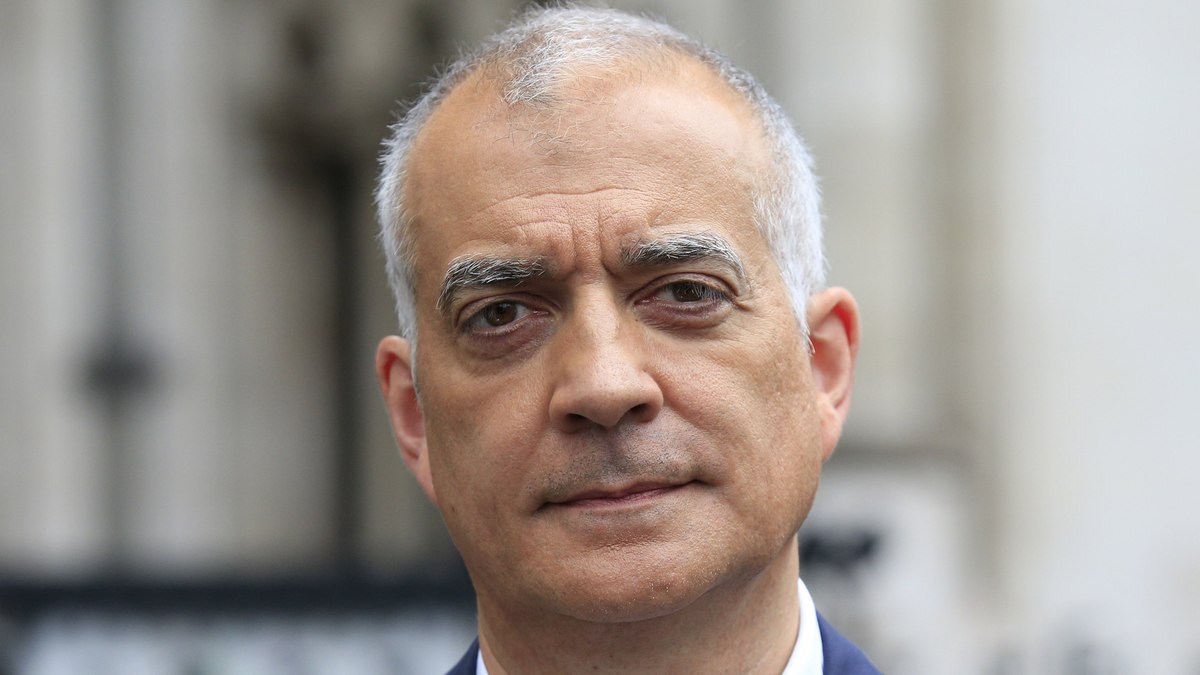
Despite the impression created by some newspaper headlines, the judge, Mr Justice Green, did not order the NHS freely to prescribe pre-exposure prophylaxis (PrEP) to all gay men who want it so that they can practise unsafe sex. He was adjudicating a much narrower legal point, which followed from the decision of the coalition government to hive off responsibility for public health from the NHS to local authorities.
The NHS, which initially said it was prepared to consider prescribing PrEP, had changed its mind because, it said, it did not have the legal right to do so and it was the responsibility of local council. This was challenged in court by the National Aids Trust and the NAT won.
NHS England said it would appeal against the ruling, but it also raised the temperature by putting out a statement that was seen as highly controversial. It said that it had to ration its spending and could not confirm funding’ for other highly expensive treatments. They include treatment for cystic fibrosis in children, low sodium levels in the blood of chemotherapy patients and brain implants for children with hearing problems. Deborah Gold, of the NAT, said it was ‘deeply unhelpful’ of NHS England ‘to be pitting PrEP against other treatments’.
However, if NHS England loses its appeal, then making a decision between providing one treatment rather than another is exactly what the NHS will have to do, simply by virtue of the fact that the NHS does not have the money to provide for free every treatment that medical science comes up with. Rationing is a fact of life in the NHS and what the judge has decided is that the NHS must include PrEP when it is calculating what it will and what it won’t prescribe.
Those who support the prescribing of PrEP say it’s pretty much an open-and-shut case. The drug has been shown to reduce the risk of transmission of HIV by around 86%. The number of new cases of HIV in Britain has been rising each year and PrEP’s success rate offers the best chance available to reverse the trend radically. They also argue that it is highly cost-effective. The treatment costs around £5,000 a year per patient. It’s reckoned that on average the treatment would need to be prescribed only for about two years to each patient, making a total cost of around £10,000 a patient. This compares with the average lifetime cost of treating someone with HIV of £360,000. Furthermore, the cost of the drug, provided by the pharmaceutical company Gilead, is likely to fall dramatically when the patent runs out in 2018.
Nonetheless, the cost to the NHS over the next couple of years of prescribing PrEP would be around £20m a year and the benefits of not having to fork out for lifetime HIV treatment would accrue only over a much longer period. So, given the cash shortage in the NHS in the immediate future, opponents argue it should concentrate its limited resources on more deserving treatments han PrEP.
At the heart of their case is the distinction they draw between illnesses that afflict people through no cause of their own and those that are the consequences of the lifestyle choices they make. In this context HIV is very much seen as an illness that is the consequence of choice: the choice of whether or not to practise safe sex. Using a condom has been shown to be the safest way to avoid the transmission of HIV and condoms are freely available on the NHS. So why, the argument goes, should the NHS spend £20m a year on a drug simply so that those who don’t like using a condom can have sex without running the risk of catching or transmitting HIV? Surely it is obvious, they say, that that £20m should be spent instead on, say, the budget for a drug that treats the faulty gene in some children with cystic fibrosis (annual cost of £182,625 per treatment).
But critics of this line of argument say that the NHS cannot start deciding whether or not to treat somebody on the basis of whether it thinks their need for treatment is the result of lifestyle choices they make. If that were the criterion, they argue, then smokers should be denied treatment when they develop lung cancer, and the obese should be turned away when they contract diabetes. The NHS has never operated on this basis, they say, and should not start to do so now.
Yet people still need to be encouraged to take responsibility for their own health and opponents of the free prescription of PrEP argue that it would actually discourage responsibility. Their case is that promiscuous gay men, the category most likely to make use of PrEP, would be liable to regard PrEP as a ‘magic pill’ protecting them from HIV. This would encourage them to abandon safe sex and throw away their condoms. But the result of this would be a rise in the incidence of other sexually transmitted diseases (putting further pressure on the NHS). Furthermore, given the fact that PrEP does not give a hundred percent guarantee of protection from HIV, its prescription, if followed by the abandonment of safe sex, could well lead to an increase in HIV, or at least to no appreciable decrease. This in turn would upturn the claim that prescribing PreP would ultimately save the NHS money.
One proposal being suggested is the American approach. PrEP should be available to anyone who wants it but they should pay for the pills themselves rather than require the NHS to pick up the tab. To many people, however, this would be yet another case of undermining the founding principle of the NHS – that treatment should be available free at the point of use.
Mr Justice Green has lobbed the decision of whether PrEP should be available free of charge back into the NHS court. What decision do you think the NHS should take?